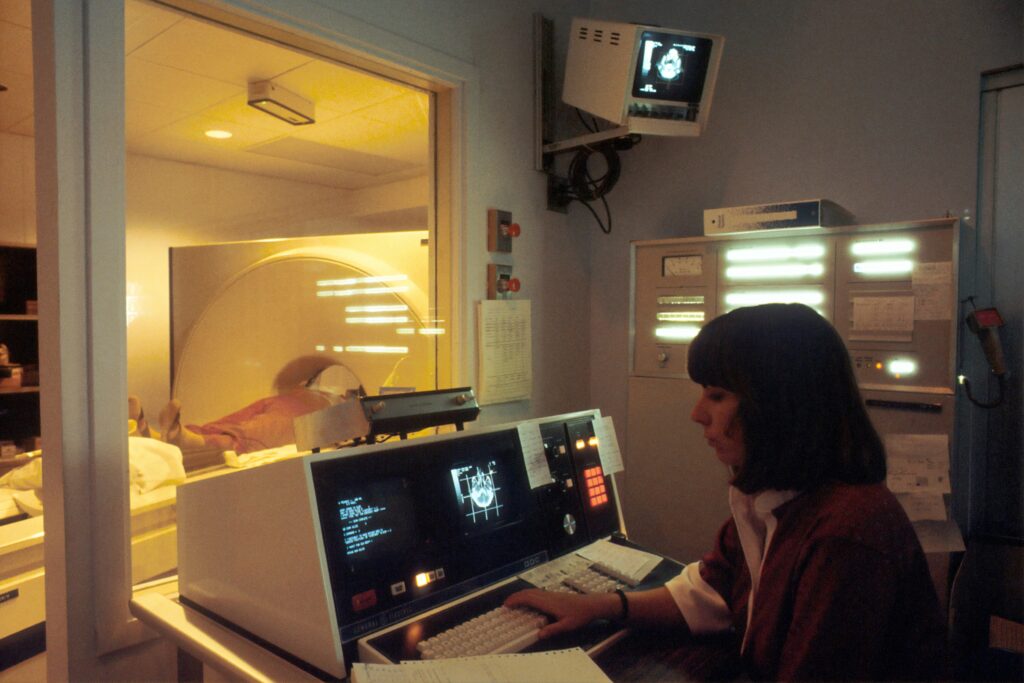
In researching and writing about trends in cancer diagnoses and outcomes, and advancements in oncology, it’s hard to do full justice to the topic. We can quote as many studies as we want, with disturbing statistics around increases in cancer occurence in the last few decades, or encouraging upticks in prognoses with improved diagnosis times and treatments. But cancer is really too visceral of a topic to adequately deal with in statistics, and too widespread and complex to fully digest in simple language.
That’s why it’s difficult to express the effect that AI tools are having on oncology. Every fraction of a percentage in a trend of earlier and more accurate diagnoses will profoundly impact peoples’ lives. Marginal growths of efficiency and accuracy – helping doctors see more patients sooner – directly cause fewer families to lose their loved ones to cancer, or give them more time with them before they do.
In 2024, scientists at the Harvard Medical School designed a versatile AI model to perform diagnostic tasks among many types of cancers. The model, called CHIEF (Clinical Histopathology Imaging Evaluation Foundation), reads digital slides of tumor tissues and analyzes them alongside a training base of over 15 million images. It achieved nearly 94% accuracy in cancer detection, outperforming other current AI approaches.
It also accurately predicted patient outcomes and long- or short-term survival. In doing so, CHIEF identified new insights around the presence of immune cells in areas of tumors – including specific characteristics of tumors that were unknown to be linked to patient survival. What if there are other, barely perceptible characteristics in the imaging we take of cancers? Important ones that researchers and oncologists might miss?
Women test for breast cancer with yearly mammograms, which are shown to help detect breast cancers early and thus greatly improve patients’ chances to beat them. Statistically, catching and treating breast cancer early is vitally important. For people with breast cancer that is localized, or hasn’t spread outside of the breast, the five-year survival rate is over 99%.
If the breast cancer is regional, having spread outside the breast to nearby structures or lymph nodes, the five-year survival rate is 87%.
If the breast cancer has spread to distant parts of the body such as the lungs, liver or bones, the five-year survival rate drops to 32%.
However, mammograms are not perfect and even patients who get them as often as recommended can run the risk of missing early warning signs. And cancer.org lists all sorts of disclaimers about what mammograms can miss. Their accuracies vary based on the researchers evaluating them, subtlety of the signs of tumors, density of the breasts being imaged, and the sometimes overwhelming volume of images to be analyzed.
Given these factors, it can take weeks for a patient to hear back about the results of a mammogram, even one with clear warning signs. This wastes precious time, and can cause patients to need more aggressive treatment. It’s a scary situation to be waiting for results from a mammogram, not sure what to think, how much to fear. It’s also extremely common.
And in many cases, breast cancer is still found less than a year after a “negative” mammogram due to technical errors, researcher errors, or non- to minimally-visible warning signs at the time of the mammogram.
Researchers have found that using AI tools to supplement mammogram analysis can flag signs of cancer – not days or weeks after a mammogram, but at the time of the appointment, while the patient is still there. This isn’t just an enhancement in efficiency; it changes the complexion of the entire process. In a study led by investigators at the UCLA Health Jonsson Comprehensive Cancer Center, researchers identified breast cancers that had been diagnosed less than a year after a negative mammogram – called interval breast cancers, or IBCs. They applied an AI tool that assigned each mammogram a likelihood of malignancy risk score from 1-10, where a score of 8-10 would be considered “flagged” as at risk for malignant cancer.
Of the 131 scored mammograms, all of which had initially come back negative, the AI model flagged 76%. Had it been available when these mammograms were originally taken, it could have immediately caught cancers that were not seen until later.
Researchers estimate, according to UCLA, that incorporating AI into breast cancer screening could help reduce IBCs by 30% – a reduction that can mean less aggressive treatments and better outcomes for patients. While AI tools don’t stand on their own to read mammograms and make diagnoses, improvements like this accelerate a long fight against cancer which has started to speed up.
And just recently, the first AI platform for breast cancer risk prediction, a tool called CLAIRITY BREAST, was approved by the FDA. This tool, developed by Clairity, can use mammograms to evaluate a woman’s risk for breast cancer in the next five years, introducing a powerful new tool to prevent cancers before they even happen or become harmful. Fighting cancer is a process that changes in nature as the cancer progresses. Dr. Connie Lehman, the founder of Clairity, is optimistic about opening up the fight to earlier stages, from detection and diagnosis to prediction and prevention.
“For more than 60 years, mammograms have saved lives by detecting early-stage cancers. Now, advancements in AI and computer vision can uncover hidden clues in the mammograms – invisible to the human eye – to help predict future risk,” she says.
This announcement from Clairity came while this article was being written. Progress in using AI for cancer detection is ramping up, and it’s almost too fast to cover. This is an exciting time, because we’re only scratching the surface of what AI can do in oncology and cancer research. Its ability to analyze images alongside databases of millions of other images, putting aside extraneous context in ways that human researchers sometimes don’t, shows incredible potential to enhance our diagnostic processes. And put into practice, percentage points of improvement – even small improvements in predicting outcomes, or catching a few more patterns that oncologists might have missed – are life changing.